Can Sitting in Traffic Give You Parkinson’s?
It’s 5 p.m. Rush hour traffic on Interstate 80 stands between you and crashing onto the couch after a long work day. The frustration of horns honking behind you, smells of old lunches, and the slow crawl home just to do it over again tomorrow is no surprise. What else could go wrong? According to a study conducted in central California, there is something else to worry about: a possible link between traffic-related air pollution and Parkinson’s disease.
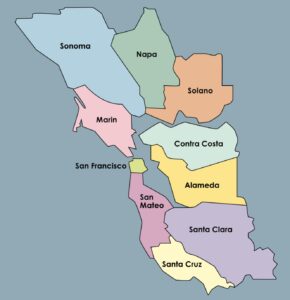
Beautiful scenery, traffic congestion, and poor air quality can go hand in hand in the Bay Area. Coastal mountain ranges in the region trap pollutants from traffic, trucks, and ports. Traffic-related air pollution contains carbon, nitrogen oxides, sulfur oxides, trace metals, and fine particulate matter.
According to the National Institute of Environmental Health Sciences, “almost 9 out of 10 people living in urban areas worldwide are affected by air pollution.” Air pollution increases risk for developing respiratory problems, cancer, cardiovascular disease, and neurological disorders.
Parkinson’s disease is a neurological disease that affects motor function. When the brain loses dopaminergic neurons, people experience tremors of the limbs and loss of movement control. Dr. Dayoon Kwon’s study explains how traffic related air pollution reduces oxygen delivery, causes inflammation to the central nervous system, and weakens the blood brain barrier. These effects provide easier access for toxins to enter the brain. Once the toxins enter the brain, an inflammatory response occurs, which plays a role in the death of dopaminergic neurons.
The study modeled the concentration of carbon monoxide and particulate matter in homes, workplaces, and traffic areas in three counties in California (Kern, Fresno, and Tulare) between 1981 and 2016. The researchers then assessed the exposure of 761 Parkinson’s patients and 910 population controls living in those areas.
The study found that long-term exposure to both traffic-related CO and particulate matter was associated with an increased risk of developing Parkinson’s, at homes and workplaces in the counties studied. When comparing exposure in workplaces and residential areas, the risk was greater for developing Parkinson’s when exposed to pollutants in workplace areas.
Other Recent Posts
Gleaning in the Giving Season
The practice of collecting food left behind in fields after the harvest is good for the environment and gives more people access to produce.
New Study Teases Out Seawall Impacts
New models suggest that sea walls and levees provide protection against flooding and rising seas with little effect on surrounding areas.
Oakland High Schoolers Sample Local Kayaking
The Oakland Goes Outdoors program gives low-income students a chance to kayak, hike, and camp.
Growing Better Tomatoes with Less Water
UC Santa Cruz researchers find the highly-desired ‘Early Girl’ variety yields more tomatoes under dry-farmed conditions.
Santa Clara Helps Homeless Out of Harm’s Way
A year after adopting a controversial camping ban, Valley Water is trying to move unsheltered people out of the cold and rain.
The Race Against Runoff
San Francisco redesigns drains, parks, permeable pavements and buildings to keep stormwater out of the Bay and build flood resilience.
Learning the Art of Burning to Prevent Wildfire
In Santa Rosa’s Pepperwood Preserve, volunteers are learning how controlled fires can clear out natural wildfire fuel before it can spark.
How does Dr. Kwon’s case study measure up to similar studies? According to Megan Maguire, EPA program analyst, “we believe this study is generally well designed with a thoughtful approach. The population case-control design is appropriate for studying Parkinson’s. There may be some differences between individuals with Parkinson’s and those serving as controls, but the authors acknowledge this and take appropriate measures (adjusting for demographic factors) to account for it.”
Has the EPA come across similar data? “Our recent assessments of the scientific evidence for particulate matter, ozone, and lead have identified some studies of air pollution and Parkinson’s, and we are continuing to evaluate this emerging literature base.”
How do genes and the environment factor into developing Parkinson’s? According to Dr. David K. Simon, a professor of neurology at Harvard Medical School, “a person without an identifiable genetic factor may have Parkinson’s if exposed to various environmental factors.” However, genes can “partially determine a person’s vulnerability to environmental agents.” (Dr. Simon was not involved in Dr. Kwon’s study.)
As the environment, and our own activities within it, become more hostile to our health, there are still ways to improve outcomes. Advocating for regulatory initiatives that focus on reducing vehicle emissions is a crucial step in making meaningful change. For policy makers, this could be providing financial incentives to businesses that focus on clean energy technologies. For the individual commuting to work, this could look like opting to ride a bike, taking public transit, and carpooling. All of which can help reduce greenhouse gases, too. A win-win for human health and climate resilience.